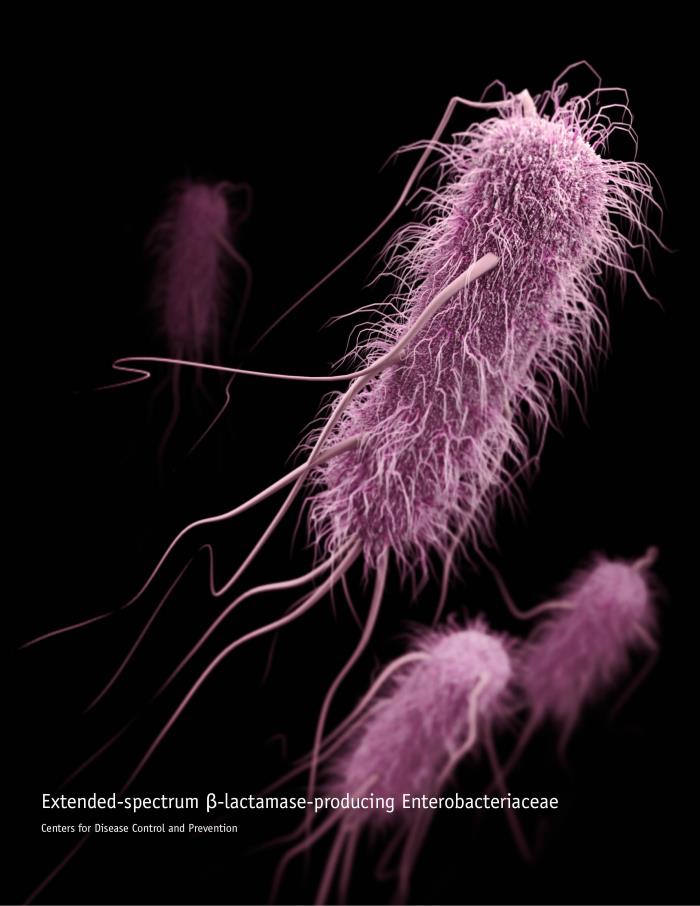
The number of infections caused by highly antibiotic-resistant extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli (E. coli) bacteria is increasing in community hospitals, a setting in which most Americans receive care, according to a new study published online Tuesday in Infection Control & Hospital Epidemiology, the journal of the Society for Healthcare Epidemiology of America.
“The lack of active screening for ESBL-producing bacteria in the majority of American hospitals means that infection prevention measures, such as contact isolation and patient cohorting, are not applied to patients who do not have symptoms, but who may be colonized with the bacteria,” said Joshua Thaden, MD, PhD, a lead author of the study and fellow in the division of Infectious Diseases at Duke University Medical Center. “These ‘silently’ colonized patients increase the risk of transmission to vulnerable patients via healthcare workers or environmental contamination, compromising safety and quality of care.”
Examining health records at 26 community hospitals in the southeastern U.S. between 2009 and 2014, researchers found that the incidence of ESBL-E. coli increased from 5.28 to 10.5 infections per 100,000 patients during that period. The number of hospitals reporting these infections also increased from 17 to 20.
“The fact that most healthcare-associated bacterial transmission events go unnoticed also means that the actual rate of bacterial acquisition may be much higher than our data suggest,” said Thaden.
Researchers found that the incidence of these particular infection strains continues to grow and surpass the presence of other bacteria, such as ESBL-producing Klebsiella pneumoniae. While the infection rate of ESBL-E. coli increased at community hospitals and health care facilities, the rate of hospital-onset infections has remained virtually unchanged.
Overall, the majority of infections caused by ESBL-E.coli occurred after exposure to the healthcare system, with nearly three-quarters of the infections either hospital-onset or healthcare-associated, making these settings focal points of transmissions. However, the study also shows a concerning rise in community-associated infections in individuals with less exposure to the healthcare system.
The retrospective study used surveillance data from the Duke Infection Control Outreach Network (DICON), and followed an earlier study of 16 hospitals that had demonstrated the emergence and rise of ESBL-E.coli infections.
Related:


2 thoughts on “ESBL-producing E. coli seen increasing in community hospitals: Study”