Ethiopia is one of three African countries reporting suspected yellow fever cases potentially linked to the Angola outbreak. According to UN health officials, the suspect cases are reported from Republic of Congo (one case), Sao Tome and Principe (two cases) and Ethiopia (22 cases).
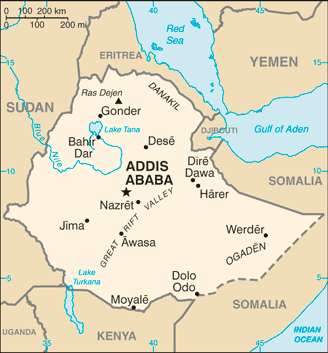
Image/CIA
Investigations are ongoing to identify the vaccination status of the cases and determine if they are linked with Angola.
In Angola, as of 1 June 2016, the country has reported 2893 suspected cases of yellow fever with 325 deaths. Among those cases, 788 have been laboratory confirmed. Despite extensive vaccination campaigns in several provinces, circulation of the virus persists.
Cunene and Malanje provinces have reported, for the first time since the beginning of the outbreak, 5 autochthonous, or locally acquired cases.
In Uganda, the Ministry of Health notified yellow fever cases in Masaka district on 9 April 2016. As of 1 June, 68 suspected cases, of which three are probable and seven are laboratory confirmed, have been reported from three districts: Masaka, Rukungiri and Kalangala. According to sequencing results, those clusters are not epidemiologically linked to Angola.
Related: Yellow fever: DRC imported cases from Angola
The World Health Organization (WHO) have the following risk assessment of yellow fever. The outbreak in Angola remains of high concern due to:
- Persistent local transmission in Luanda despite the fact that approximately eight million people have been vaccinated.
- Local transmission has been reported in ten highly populated provinces including Luanda. Luanda Norte, Cunene and Malenge are the provinces that most recently reported local yellow fever transmission.
- The continued extension of the outbreak to new provinces and new districts.
- High risk of spread to neighbouring countries. As the borders are porous with substantial crossborder social and economic activities, further transmission cannot be excluded. Viraemic travelling patients pose a risk for the establishment of local transmission especially in countries where adequate vectors and susceptible human populations are present.
- Risk of establishment of local transmission in other provinces where no autochthonous cases are reported.
- High index of suspicion of ongoing transmission in hard-to-reach areas like Cabinda.
- Inadequate surveillance system capable of identifying new foci or areas of cases emerging.
Related:
- E. coli outbreak: 38 people sickened in 20 states, Linked to potentially tainted flour
- Dengue fever reported in traveler to Key West, Locally acquired case
- Ebola virus Triage Test gets FDA Emergency Use Authorization


2 thoughts on “Ethiopia: 22 suspected yellow fever cases being investigated”