In a follow-up on the hepatitis A outbreak in Indiana, health officials have reported 283 outbreak cases since Nov. 2017, including one death. Of the outbreak cases, 47 percent required hospitalization.
Indiana has an average of 20 cases of hepatitis A per 12 month period.
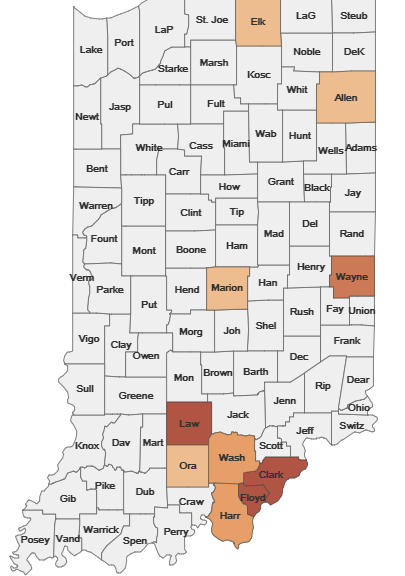
Counties in the southern part of the state have been hit hardest–Clark (65) and Floyd and Lawrence counties with 43 cases each. Cases have been infected with acute hepatitis A virus (HAV) strains genetically linked to outbreaks across the United States.
Transmission is presumed to occur person to person; no contaminated commercial food product has been identified. Based on CDC guidelines, populations who are homeless, transient, incarcerated or use illicit drugs and their close direct contacts are considered at increased risk of exposure to hepatitis A.
To reduce the risk of hepatitis A transmission, people who have not received two doses of hepatitis A vaccine may ask their healthcare providers for protection. Additionally, always wash your hands with soap and water after going to the bathroom, after changing diapers and before preparing meals for yourself and others. Do not attend work or school if you are experiencing symptoms of hepatitis A, which include nausea, vomiting, diarrhea, loss of appetite, tiredness, stomach ache, fever, dark-colored (cola) urine, light-colored stool and jaundice (yellowing of skin and eyes). Symptoms may take as many as 50 days from exposure to appear.
- DR Congo: Epidemiological vigilance needed to prevent recurrent Ebola outbreaks
- Cyclospora cases multiply in Illinois
- Tick-borne disease: Indiana reports rise in cases including ehrlichiosis fatality
- Malaysia hand, foot and mouth disease cases top 35,000; Prompts interagency cooperation
- Pepperidge Farm Goldfish crackers recalled: Potential for Salmonella


