New evidence from Princeton University suggests that Pseudomonas aeruginosa, a pathogenic microorganism that has become resistant to many antibiotics, derives its pathogenicity from a previously unknown sense of touch, paving the way for new classes of targeted antibiotics.
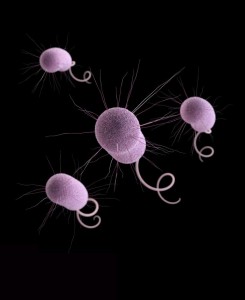
P. aeruginosa is a Gram negative aerobic commensal bacteria present on many individuals, but is an opportunistic pathogen infecting immunocomprised individuals or gaining access to the body through cuts and surgeries. P. aeruginosa is able to live in and on plants, animals, and other natural and synthetic locales; this ubiquity in location drove researchers from Princeton to determine how this bacteria attaches to multiple surfaces so successfully.
Like many pathogenic microorganisms, P. aeruginosa has long been known to form biofilms on surfaces. These biofilms provide bacteria a protective niche from a hostile environment (intestinal acids, antibiotics, weather conditions, etc.), and allow communication (“quorum sensing”) within the community for enhanced growth and pathogenesis. Most bacteria use quorum sensing to tell their comrades that a specific site is hospitable for growth, but P. aeruginosa latches on to any surface it contacts independent of quorum sensing and immediately begins pathogenic biofilm formation.
The researchers believed this attribute is due to a P. aeruginosa membrane protein that facilitates attachment, signaling to the bacteria that it is present on a surface and may commence growth. Through microarray analysis and targeted mutations of P. aeruginosa surface moieties, the team discovered that PilY1, a surface protein homologous to eukaryotic surface mechanotransducers, is the key player in regulating P. aeruginosa attachment and subsequent virulence.
P. aeruginosa was allowed to grow uncontested on a variety of surfaces, including plants, animal and amoeba cells, and in a regular culture dish. In wild type cells, P. aeruginosa instinctively formed a biofilm when a new surface was added to culture. In P. aeruginosa that had PilY1 deleted or mutated, the cells grew, but much more slowly and did not develop pathogenic biofilms. Key virulence factors were also downregulated, showing that PilY1 activation is the beginning signal of a virulence pathway.
“I’m very optimistic that we can use drugs that target PilY1 to inhibit the whole virulence process instead of killing off bacteria piecemeal,” said corresponding author Zemer Gitai, a Princeton associate professor of molecular biology. Antibiotics today mainly attack intracellular bacterial proteins and gene networks. Bacteria then evolve ways to pump the antibiotic out before it becomes effective, rendering the antibiotic useless and the bacteria resistant. By inhibiting an extracellular protein used for attachment, bacteria will not be able to adhere to any surface in the body and will be shed or excreted with no ill effects.


Fascinating breakthrough! But be careful.
Dr Gitai notes that “By inhibiting an extracellular protein used for attachment, bacteria will not be able to adhere to any surface in the body and will be shed or excreted with no ill effects.”
But attachment by pathogenic bacteria is the same process whereby marine bacteria attach to surfaces such as eelgrass fronds, providing a substrate for mussel larvae to land on and consume – acquiring their shells in the process. Other marine bacteria regulate the level of CO2 in our oceans by attaching to carbon particles; then, once a quorum is reached, digesting it en masse.
For that matter, sewage treatment plants rely on bacteria latching onto and breaking down human wastes.
We want to be very careful to avoid suppressing these healthy natural processes of non-injurious bacteria – which are of course the overwhelming majority of bacteria. In communities whose sewage plants pump into the sea, heavy use of such medicines could be problematic!
Caution, please!
Ron Huber, executive director
Friends of Penobscot Bay,
Rockland Maine