In an update to a report yesterday, the UCLA Health System notified 179 patients on Feb. 18 that they may have been exposed last fall to the carbapenem-resistant enterobacteriaceae (CRE) bacteria during an endoscopic procedure to diagnose and treat diseases of the liver, bile ducts and pancreas at Ronald Reagan UCLA Medical Center. A total of seven patients were infected; the infection was a contributing factor in the death of two patients.
Only patients who underwent these endoscopic procedures from October 3 to January 28 are at risk of infection. Those patients are being offered a free home testing kit for analysis at UCLA to determine if they carry the bacteria in their intestines.
UCLA followed both national guidelines and the sterilization standards stipulated by Olympus Medical Systems Group, the instrument’s manufacturer. However, an internal investigation determined in late January that CRE may have been transmitted by two of the seven Olympus scopes used by the hospital during the four-month period.
UCLA immediately began reviewing every patient record to determine which patients underwent the procedure using this type of scope between October and January. In an abundance of caution, the hospital has notified all 179 patients who were examined with one of the seven instruments during that time.
Related: FDA issues safety alert about ERCP endoscopes cleaning after UCLA outbreak
The two infected scopes were immediately removed from use for return to Olympus. UCLA currently performs a more stringent decontamination process that exceeds both the manufacturer’s standards and national guidelines. Hospital staff thoroughly clean the instrument and place it in an automated machine for disinfection. Then the instrument is sent off-site for a second sterilization process using a gas called ethylene oxide.
In a press briefing in 2013, CDC director, Dr. Thomas Frieden said the following about CRE:
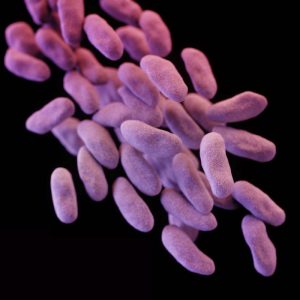
What I’m talking about today is CRE, carbapenem-resistant enterobacteriaceae. CRE are nightmare bacteria. They pose a triple threat. First, they’re resistant to all or nearly all antibiotics. Even some of our last-resort drugs. Second, they have high mortality rates. They kill up to half of people who get serious infections with them. And third, they can spread their resistance to other bacteria. So one form of bacteria, for example, carbapenem-resistant klebsiella, can spread the genes that destroy our last antibiotics to other bacteria, such as E. coli, and make E. coli resistant to those antibiotics also.
To give you some background, the long word, carbapenem-resistant enterobacteriaceae, is a family of more than 70 different kinds of bacteria. It includes some very common ones, like klebsiella and E. coli, that are normally present in our intestines. Sometimes, however, these bacteria can get into the wrong places like the blood or the bladder. When this happens, people can get severe infections called urinary tract infections. Some types of enterobacteriaceae have become resistant to antibiotics, even high-powered, last resort, last line of defense of antibiotics, called carbapenems. Antibiotic resistance is what turns normal enterobacteriaceae into drug resistant or CRE. Now there are many different types of resistance that are carried by different plasmids that go by names like KPC or VIM or NDM, or CRKP. These are all types of CRE. Types of resistant bacteria. They all result in the same end point, a highly drug-resistant infection that has a very high fatality rate for people who have serious infections with it.
The risk of CRE infection is highest among patients who are getting complex or long-term medical care. This mostly means patients in regular hospitals or long-term acute care hospitals, or nursing homes. CRE spread among people, mostly patients in hospitals and long-term care facilities, usually from unclean hands. Medical devices such as ventilators or catheters increase the risk of life-threatening infection because they allow new bacteria to get deeply into a patient’s body.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS


2 thoughts on “UCLA outbreak update: CRE ‘contributing factor’ in the death of two patients”