Back in 2010, researchers from the United Kingdom were talking about an enzyme known as NDM-1 (New Delhi metallo-β-lactamase 1), that has found its way from the Indian subcontinent and could potentially become a major global health problem.

The enzyme is carried in certain gram negative bacteria like E. coli and Klebsiella, and makes the bacterium resistant to the carbapenem class of antibiotics.
The carbapenems are broad spectrum antibiotics used to treat various infections, including difficult to treat infections. They are typically highly resistant to beta lactamases. Beta lactamases are enzymes carried in certain bacteria that make the bacteria resistant to beta-lactam drugs like penicillin.
Last summer, Washoe County health officials in Reno, Nevada reported on a patient who, in a wound culture sample, tested positive for a carbapenem-resistant Enterobacteriaceae (CRE) Klebsiella pneumoniae.
The sample was sent to the Centers for Disease Control and Prevention (CDC), which confirmed the presence of New Delhi metallo-beta-lactamase (NDM) as the mechanism of antimicrobial resistance, according to a Morbidity and Mortality Weekly Report (MMWR) report published Friday.
According to the report:
The patient was a female Washoe County resident in her 70s who arrived in the United States in early August 2016 after an extended visit (2 years) to India. She was admitted to the acute care hospital on August 18 with a primary diagnosis of systemic inflammatory response syndrome, likely resulting from an infected right hip seroma. The patient developed septic shock and died in early September. During the 2 years preceding this U.S. hospitalization, the patient had multiple hospitalizations in India related to a right femur fracture and subsequent osteomyelitis of the right femur and hip; the most recent hospitalization in India had been in June 2016.
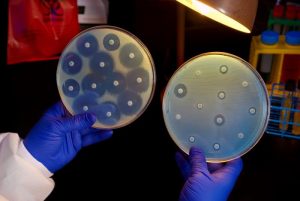
Antimicrobial susceptibility testing in the United States indicated that the isolate was resistant to 26 antibiotics, including all aminoglycosides and polymyxins tested, and intermediately resistant to tigecycline (a tetracycline derivative developed in response to emerging antibiotic resistance). Because of a high minimum inhibitory concentration (MIC) to colistin, the isolate was tested at CDC for the mcr-1 gene, which confers plasma-mediated resistance to colistin; the results were negative. The isolate had a relatively low fosfomycin MIC of 16 μg/mL by ETEST. However, fosfomycin is approved in the United States only as an oral treatment of uncomplicated cystitis; an intravenous formulation is available in other countries.
Surveillance was conducted among patients admitted to the same unit as the patient and no CRE was detected.
This report highlights three important issues in the control of CRE. First, although CRE are commonly sent to CDC as part of surveillance programs or for reference testing, isolates that are resistant to all antimicrobials are very uncommon. Among >250 CRE isolate reports collected as part of the Emerging Infections Program, approximately 80% remained susceptible to at least one aminoglycoside and nearly 90% were susceptible to tigecycline.
Second, to slow the spread of bacteria with resistance mechanisms of greatest concern (e.g., gene encoding NDM or mcr-1) or with pan-resistance to all drug classes, CDC recommends that when these bacteria are identified, facilities ensure that appropriate infection control contact precautions are instituted to prevent transmission and that health care contacts are evaluated for evidence of transmission.
Third, the patient in this report had inpatient health care exposure in India before receiving care in the United States. Health care facilities should obtain a history of health care exposures outside their region upon admission and consider screening for CRE when patients report recent exposure outside the United States or in regions of the United States known to have a higher incidence of CRE.
Related:
- mcr-1 gene: An interview with Dr Judy Stone
- CDC on the first mcr-1 gene in E. coli bacteria found in a human in the US
- European Medicines Agency looks at colistin use in animals following mcr-1 gene discovery


It’s not resistant to allicin you dumb f**cks.
I’m not familiar with allicin. So, you’re saying that this is not (so far) likely to evolve into a doomsday pandemic?