The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has adopted a positive scientific opinion of fexinidazole, the first all-oral treatment that has been shown to be efficacious for both stages of sleeping sickness. This approval is a result of clinical trials led by the non-profit research and development organization DNDi and an application submitted by Sanofi. The decision paves the way for the distribution of fexinidazole in endemic countries in 2019.
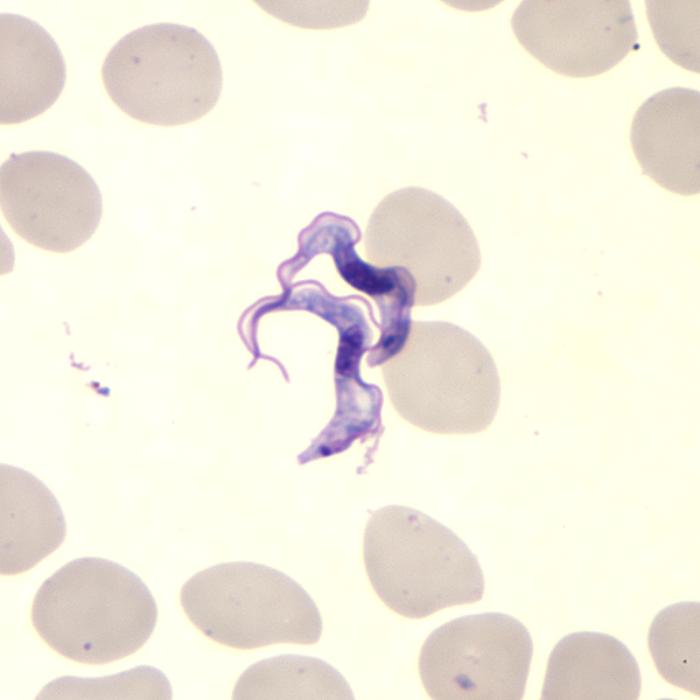
Sleeping sickness, or human African trypanosomiasis (HAT), is usually fatal without treatment. Transmitted by the bite of a tsetse fly, it causes neuropsychiatric symptoms; including aggression, psychosis, and a debilitating disruption of sleep patterns that have given this neglected disease its name. About 65 million people in sub-Saharan Africa are at risk.
“I’ve dedicated my life as a doctor to sleeping sickness. An all-oral treatment has been a dream of mine for decades. Those affected are some of the most vulnerable and live in some of the most remote areas of the Congo, if not the world. They need a treatment that is safe, effective and simple,” said Dr Victor Kande, who as Neglected Tropical Diseases Expert Advisor to the Ministry of Health of the Democratic Republic of Congo (DRC), was the principal investigator of the trials. “Less than ten years ago we were still treating this disease with an arsenic derivative that killed 5% of all patients. While current treatments are safe and effective, they require a patient to be hospitalized and pose a huge logistical burden on the health system. Fexinidazole comes as a simple pill: this is a huge leap in how we can tackle this deadly disease.”
Fexinidazole is indicated as a 10-day once-a-day treatment for Trypanosoma brucei gambiense sleeping sickness (the most common form of the disease, found in West and Central Africa). Importantly, fexinidazole is the first all-oral treatment that works both for (i) the early stage of the disease as well as the (ii) second stage of the disease in which the parasites have crossed the blood-brain barrier, causing patients to suffer from neuropsychiatric symptoms.
African sleeping sickness: A short Q&A with an ID physician
During the clinical trials, which enrolled 749 patients in the DRC and Central African Republic, fexinidazole showed high efficacy and safety in both stages of the disease, both in adults and children ≥ 6 years old and weighing ≥ 20 kg. Results showed that fexinidazole could, therefore, eliminate the need for systematic hospitalization and lead to a potential reduction in the number of lumbar punctures.
“Fexinidazole is an entirely new chemical entity that has been developed through an alternative non-profit R&D model. It is the first new chemical entity to be developed by DNDi,” said Dr Bernard Pécoul, DNDi Executive Director. “This therapeutic breakthrough is testament to the unique partnership between DNDi and Sanofi to discover, develop, and register a treatment for a severely neglected disease.”
Fexinidazole is a 5-nitroimidazole derivative that was rediscovered in 2005, through collaboration with the Swiss Tropical and Public Health Institute, during DNDi’s search for compounds with anti-parasitic activity, after being developed and then abandoned for strategic reasons by Hoechst (now Sanofi) in the 1980s. In 2009, DNDi and Sanofi concluded a collaboration agreement for the development, manufacturing, and distribution of fexinidazole, with DNDi responsible for pre-clinical, clinical, and pharmaceutical development, and Sanofi for industrial development, registration, production, and distribution of the drug.
“This therapeutic breakthrough is the latest milestone in Sanofi’s long-term commitment to sleeping sickness,” said Dr Ameet Nathwani, Chief Medical Officer and Executive Vice President Medical Function. “Fexinidazole is the proof that partnerships between public and private sectors can deliver safe and effective medicines for the most neglected patients. Sanofi is proud to donate this medicine to the World Health Organization as part of our mission to support the elimination of sleeping sickness.”
In December 2017, Sanofi submitted a regulatory dossier to the European Medicines Agency under Article 58 of Regulation 726/2004, an innovative regulatory mechanism intended for the review of new medicines destined for use outside of the European Union. By allowing for the participation of endemic countries (DRC and Uganda) and of the WHO in the evaluation of the fexinidazole regulatory dossier, approval under Article 58 also facilitates and could accelerate future national product registrations and patient access.
“Together with Ministries of Health in endemic countries we have shown it is possible to conduct high quality trials in the most challenging settings,” said Dr Nathalie Strub-Wourgaft, DNDi Director of Neglected Tropical Diseases. “This is only the first step – we now need to ensure patients can access and benefit from this new drug.”
To develop fexinidazole, DNDi spent EUR 55 million (USD 62.5 million), which includes costs related to pre-clinical development and clinical studies. The project was supported by seven European countries (France, Germany, the Netherlands, Norway, Spain, Switzerland, and the UK) as well as private donors including the Bill & Melinda Gates Foundation and Médecins Sans Frontières.
The majority of sleeping sickness patients are reported in the Democratic Republic of Congo, where 78% of Trypanosoma brucei gambiense sleeping sickness cases were reported in 2017, followed by the Central African Republic, Guinea, and Chad. The latest data released by the WHO in July 2018 confirm a sustained decrease in the number of new cases. Only 1,447 new cases were reported to the WHO in 2017 compared to 2,164 cases in 2016 and 9,870 cases in 2009. But the history of sleeping sickness is marked by resurgence, interspersed by decades where the disease has seemed largely under control. In its roadmap on neglected tropical diseases published in 2012 and supported the same year by the London Declaration, the WHO identified sleeping sickness as a public health problem, and targets its elimination by 2020.