The number of plague cases are closing in on 700 cases, according to the latest World Health Organization (WHO) update. Between 1 August and 12 October 2017, a total of 684 cases (suspected, probable and confirmed) including 57 deaths (case fatality rate 8.3%) have been reported from 35 out of 114 districts in the country.
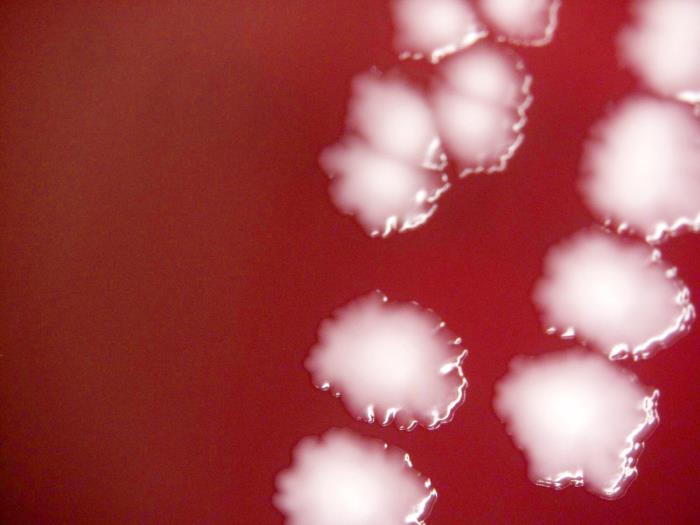
Image/CDC
Of these, 474 cases (69.3%) were clinically classified as pneumonic plague, 156 (22.8%) were bubonic plague, one case was septicaemic plague, and 54 cases were unspecified. At least fifteen healthcare workers have contracted plague since the beginning of the outbreak.
Concerning the susceptibility to antibiotics, the Pasteur Institute Madagascar reports:
Monitoring the susceptibility of strains of Yersinia pestis to different antibiotics (ATB) is a priority for the success of the National Program for the Control of Plague.
It detects the emergence of strains of reduced susceptibility or resistance to Streptomycin (Sm) and Sulfamides (Sxt), antibiotics recommended and used in the National Program and to evaluate other alternatives (Tetracycline (Tet) , Ciprofloxacin (Cip), Chloramphenicol (Chl)) for treatment.
Since the beginning of the season, the 11 isolated strains are sensitive to these ATBs. They are from Miarinarivo, Moramanga, Mahajanga, Tsiroanomandidy and Andramasina.
Plague is known to be endemic on the Plateaux of Madagascar (including Ankazobe District where the current outbreak originated) and a seasonal upsurge (predominantly the bubonic form) usually occurs early every year between September and April. Unlike the usual endemic pattern, the plague season began early this year, and the current outbreak has affected major urban centres, including Antananarivo (the capital city) and Toamasina (the port city).
Related:
- Nigeria: Lymphatic filariasis eliminated in Plateau and Nasarawa states
- Human Usutu virus infections are more prevalent than previously thought
- Plague treatment center deployed to Madagascar
- Plague death toll now 57, 10 million Euros needed in outbreak battle
- Sydney: Hepatitis A issued for patrons of Sokyo restaurant
- Canada: Increase of invasive Group A Strep reported in Thunder Bay


Once pneumonic plague becomes resistant to antibiotics that’s it. The end of cramped, overcrowded cities around the world.
When are countries going to bar flights to and from Madagascar. The lack of any action will see this disease take a one way flight ticket to neighbouring countries, as it has done with the Seychelles. Whose next South Africa?
losses of disseminated plague make any and all such expenses imperative.
Remarkably the world health organization’s recommendations regarding travel and exchange in Madagascar are,as of this date, without restriction.
The single most effective and prudent protective measure in epidemics is isolation and avoidance of infected persons.
Just as in the Ebola epidemic in eastern Africa, the organizations charged with controlling outbreaks and protecting the world’s population completely discard the most effective and reasoned intervention.
Medically efforts to isolate and/or quarantine infected, or possibly infected, persons is unquestionably desirable and in the world communities interest.
It is discouraging, worrisome, and inexplicable that in an age where air traffic exponentially increases the risk of epidemic spread, no recommendations or utilization of isolation and/or pointing are mentioned.
The Ebola epidemic luckily did not expand, despite travel risk assessments that were meaningless, in large part due to the poverty of the countries and their citizens. The East Africa Ebola epidemic differentially infected the poorest of those in the involved countries and the lack of significant respiratory spread kept the disease relatively limited to those poverty-stricken population. The result being that overwhelmingly the infected individuals were not persons that had access or habit of air travel.
With the development of pneumonic spread in Madagascar it could be anticipated that a broader population involvement is likely.
The potential for air travel and dissemination of pneumonic plague to other countries is nightmarish to consider.
I hope and pray that this epidemic can be contained. I do not understand the limited strategy identified by the world health organization and others.
I fear that the lessons that should have been more learned with Ebola and East Africa were not.
Isolation and/or quarantine are no doubt expensive, difficult, and involve major political and economic challenge-despite these costs the potential losses of disseminated plague make any and all such expenses imperative.