University of KwaZulu-Natal (UKZN) researchers have published details of a new malaria diagnostic test which detects a new form of malaria: Plasmodium knowlesi (P. knowlesi).
The College of Agriculture, Engineering and Science’s Professor Dean Goldring, conducted the research with Dr Robert Krause, who did the investigations as part of his PhD thesis. “This is the first test that can detect a unique protein from the parasite using an antibody,” said Goldring. “We have identified a unique malaria protein called PMT, short for phosphoethanolamine-N methyl transferase.
“The protein is not made by human cells – we have made antibodies against the protein. Our antibodies can detect this protein and by detecting the protein, distinguish between different species of malaria,” he said.
According to the World Health Organisation, 1.4 billion people are at risk of contracting the disease and there are 1.5 million cases recorded in South-East Asia, the region affected by this strain of malaria.
Goldring outlined the significance of the breakthrough: “There are other antibody protein combinations in tests that are used to detect Plasmodium falciparum (P.falciparum) malaria and other malaria infections. The existing tests do not identify P. knowlesi malaria or distinguish this malaria from other malaria species. Our test is the first of its kind to detect P. knowlesi malaria using an antibody/protein combination,” he said.
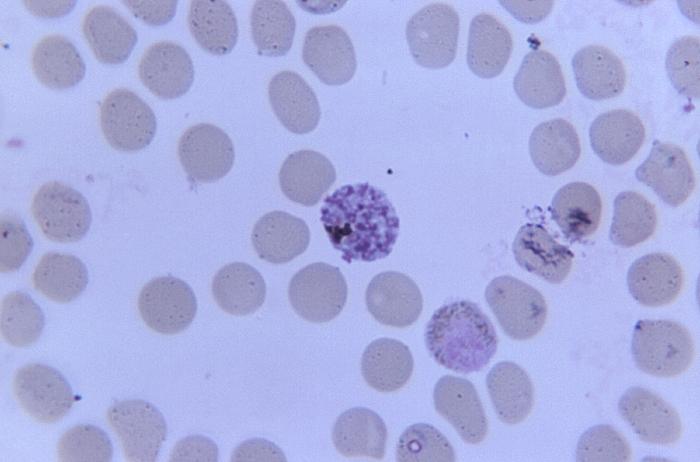
“P. knowlesi malaria, known as monkey malaria, was not thought to infect humans. P. knowlesi malaria parasites when stained in a patient’s blood and viewed under the microscope look very much like P. falciparum malaria parasites. Microscopy is the traditional method to diagnose malaria and has worked very well over the last hundred years,” he said.
Goldring’s interest in malaria was sparked from him having contracted the disease as a child. “I was brought up in Malawi and had malaria several times. I was fortunate as the drug chloroquine was very effective at the time. I wanted to do something to help kids who got malaria.”
He has studied malaria vaccines in the United States and cerebral malaria in children in the United Kingdom.
P. knowlesi malaria is not found in South Africa so arrangements are being made with associates in Malaysia to obtain samples for extensive testing. “Once we have sufficient evidence from experiments in our laboratory, we would like to see if our antibody/protein combination can be used in a point of care diagnostic dipstick-based test,” said Goldring. “These tests use a small sample (drop) of blood which is mixed with detecting reagents and added to a test strip. The samples are carried along the test strip by capillary action. Lines appear on the strip, one to show that the test works and a second line indicates the presence of malaria.”
Goldring explained further benefits of the research: “The most popular antibody/protein combination to detect malaria detects a unique P. falciparum protein called PfHRP2. Unfortunately, there is an increasing number of P. falciparum malaria parasites that no longer make the protein PfHRP2 and therefore the test based on detecting PfHRP2 is no longer reliable in some locations such as Peru. There have also been reports of the test not working in some places in Africa. The protein we have identified can also be used to detect a P. falciparum infection.
“We have also found antibody/protein combinations that can detect Plasmodium vivax malaria (another strain of the disease). The current malaria antibody/protein tests do not work well when stored at the high ambient temperatures found in many malaria endemic regions. We are working on ways to improve the thermal stability of the reagents in tests and ways to improve the tests to be able to show whether a patient has many or a few parasites in their blood.”
In 2004 Professor Balbir Singh, a colleague Goldring worked with several years ago, showed that P. knowlesi malaria infects humans and is widespread in Malaysia. Singh also showed that a P. knowlesi infection can be misdiagnosed as a P. falciparum infection. “This is important as the drug regime to treat P. falciparum and P. knowlesi malaria are different. Correct diagnosis of a P. knowlesi infection in some areas is thought to have contributed to a significant reduction in the case fatality rates. P. knowlesi parasites divide very quickly (every 24 hours) in red blood cells and so the disease can rapidly develop from an uncomplicated to a severe infection in a patient,” said Goldring.
Goldring, who has worked at UKZN for 19 years, holds degrees from the University of Dundee in Scotland and the University of Zimbabwe. He enjoys teaching and believes “a university environment is an excellent place to do research and teaching and where I can integrate my research into my teaching”.
The research was funded by UKZN, the National Research Foundation and the Medical Research Council of South Africa.
Related:

