By Glenn Laverack, PhD
The ongoing pandemic of the COVID-19 coronavirus is the largest since the ‘Spanish Flu’ 100 years ago and probably the single largest public health intervention ever. Until an effective vaccine or treatment is available the coronavirus can only be halted by enabling people to take more control over their lives, individually and collectively, and on a global scale. In an infectious disease outbreak, the first enemy is time. Most governments have responded quickly to enforce lock-downs and to use communication and moral suasion to influence individual risk behaviours such as social distancing. The outbreak response has been driven by data, by difficult political decisions and to some extent, by what works in public health. In truth, we have underestimated COVID-19 which has overwhelmed healthcare systems and has pushed hard working health professionals to the limit. The pressure has revealed gaps in risk communication, community involvement, protective equipment, critical care and testing.
In an infectious disease outbreak, the first enemy is time
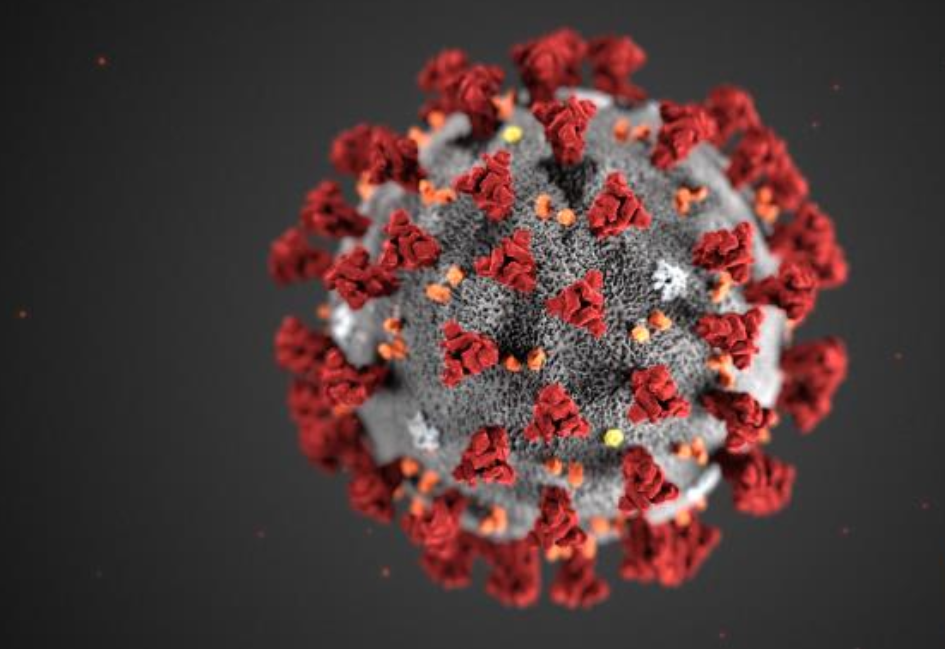
COVID-19 is ‘Disease X’, a relatively unknown pathogen leading to a pandemic, originating as a zoonotic virus and with a high rate of infection. Similar disease outbreaks include the Severe Acute Respiratory Syndrome (SARS) in 2002 and the Middle East respiratory syndrome–related coronavirus (MERS-CoV) in 2018. All have occurred in Asia and have resulted from the sale and preparation of wild animals under unregulated and/or insanitary conditions, creating an opportunity for the transmission of a virus (Laverack, 2018). Why have international public health authorities continued to allow these conditions to persist? The real surprise about COVID-19 has been the rapid spread and severity, leaving us unable to predict how it will develop within societies. The nature of COVID-19 has created a sense of fear and a need to act urgently and without precedent. Some decisions will leave behind long-lasting human and economic costs that will be deeply felt in society. Next time, if we can choose, will we want to use such draconian measures to halt the outbreak or will we choose to use a more nuanced public health response?
COVID-19 will leave behind long-lasting human and economic costs that will be deeply felt
There is not a single model for communication and community engagement during a pandemic. Each country must develop its own approach based on the strengths and weaknesses of its socio-cultural, political, economic, infrastructural and historical context. Some socio-cultural contexts, for example, can tolerate long-term lock-downs whilst others will resist, especially as life becomes increasingly more difficult. What works in some countries has to be treated with caution because it may not be possible to replicate in other countries.
Each country must develop its own approach for community engagement and communication based on its strengths and weaknesses
Governments have not widely used community-centred approaches, although there is no excuse not to actively involve people in an outbreak response. The emphasis has been on individual compliance and, in particular, on strict population control measures. Health promotion has an important role in changing behaviours such as hand-washing as well as to strengthen community involvement. Communities can monitor the everyday movement of people in a given locality such as a neighbourhood, a village or across borders. Community self-management can ensure compliance with the requirements of a lock-down by helping others to understand the consequences of their actions and to report violations or suspected cases (Laverack and Manoncourt, 2015). Lock-downs have a greater chance of success if people are enabled to take more control and responsibility and are motivated by a sense of altruism, rather than by imposing punishment for violations. In the Ebola Virus Disease outbreak in West Africa, non-compliant behaviours were observed during lock-downs, sometimes made worse by poor service delivery, weak information flow and a lack of government support to the vulnerable. The situation worsened as the lock-downs continued, often in specific localities and attempts by the security forces to coerce communities to comply were counterproductive and led to mistrust and escalated resistance (Laverack, 2018, Chapter 9).
There is no excuse not to actively involve communities in a disease outbreak response
The protection of the vulnerable in society has not been fully addressed during the pandemic including refugees and migrants, the socially isolated, the homeless, elderly people in residencies, the mentally ill and women and children at risk from domestic violence. People who are vulnerable and who suffer inequality will be more adversely affected by COVID-19. Similarly, those countries with the greatest inequalities will potentially be more adversely affected by COVID-19. Overcrowded and slum conditions with insufficient water supply and poor sanitation and a high population density deny the opportunity for proper hygiene and social distancing. The local administrative and enforcement authorities, health agencies and communities must work together to address an outbreak but small gains have been made on how to reach slum communities, with no clear strategy for cooperation, engagement and communication (Laverack, 2018a).
People who are vulnerable and who suffer inequality will be more adversely affected by COVID-19
The mobilization of volunteers during the pandemic by non-government agencies, universities and community-based organisations has provided much needed support for, example, to deliver essential items, for making face masks and checking on vulnerable people. The usual social support network of friends and family is broken during a lock-down and people within apartment blocks, neighbourhoods and villages have had to help one another. However, altruism has not been universal, with some localities being better organised and more supportive than others. The pre-planning for, and the support of, community based organisations and voluntary support networks by the government is good practice because this provides a link between people affected by COVID-19 and services. However, the support should be systematic to ensure that all vulnerable people are helped during an outbreak.
Governments should use a systematic approach to help the vulnerable during an outbreak
Health promotion activities must be maintained during a pandemic to support a healthy physical, mental and spiritual lifestyle, especially during confinement. Places of worship have been closed, despite the ease of social distancing, and people are leading stressful and sedentary lives. Promoting a healthy lifestyle would include reinforced messaging about healthy eating and activity levels, stress reduction and safe alcohol and tobacco use at home. It is also important that information is made available about ongoing prevention programs such as vaccination and screening and for online and telephone services to cope with stress and domestic violence. In West Africa, untreated malaria cases and unvaccinated children for diseases such as measles were estimated to have led to the death of more people than the actual Ebola Virus Disease outbreak (Roberts, 2015). Health promotion messaging can also help to counter false information and rumours, to reduce stigma and to mitigate public mistrust about public health services.
Health promotion activities must be maintained during confinement to support a healthy physical, mental and spiritual lifestyle
Communities must be an intrinsic part of an outbreak response including during the exit strategy from lock-downs. Everyone must be actively involved in order for the response to be successful. Community engagement and communication are two important approaches that can enable people to take more control of their lives and health. However, communities and community-based organisations must receive government resources to strengthen social networks and local capacity to address an outbreak. Not to do so is questionable and the reasons for not actively involving communities in an outbreak response must be assessed, including any assumptions about weak local competencies and the lack of trust between government and civil society.
Glenn Laverack, Visiting Professor, Department of Sociology and Social Research, University of Trento, Italy
References
Laverack, G. (2018) Health promotion in disease outbreaks and health emergencies. Boca Raton, Florida. CRC press. Taylor & Francis group.
Laverack, G. (2018a) Blacker than Black: Failing to Reach Slum Communities in Disease Outbreaks. Infect Dis Immunity. Vol 1 (1):4-6.
Laverack, G. and Manoncourt, E. (2015) Key experiences of community engagement and social mobilization in the Ebola response. Global Health Promotion. 1757-9759. Vol (0): 1-4.
Roberts, L. (2015). As Ebola fades, a new threat. Science 347(6227): 1189.


One thought on “Communities and COVID-19: Perspectives from a health promotion expert”