Leading food safety consultancy STS has conducted extensive research on behalf of the Food Standards Agency (FSA), which included examining 10 listeriosis outbreaks in hospitals, almost all of which were linked to consumption of pre-packed sandwiches. This article uses these results to consider the threat posed by listeriosis and offers preventative measures.
Listeriosis – the killer pathogen is on the rise
It may come as a surprise to learn that listeriosis leads to more fatalities than any other foodborne illness in the UK. Although incidences of listeriosis are relatively low compared to other food-related pathogens, its fatality rate can be about 25 to 30 per cent, costing the UK economy an estimated £245 million per year. Public Health England reports1 that the number of cases of listeriosis in England and Wales have increased by 23 per cent in past decade (2005 – 2014) compared to the previous one (1995 – 2004). In Europe, cases of listeriosis have been increasing over the past five years with an 8.6 per cent rise between 2012 and 20132, according to the European Food Safety Authority. Most fatalities are among the elderly and those with weakened immunity.
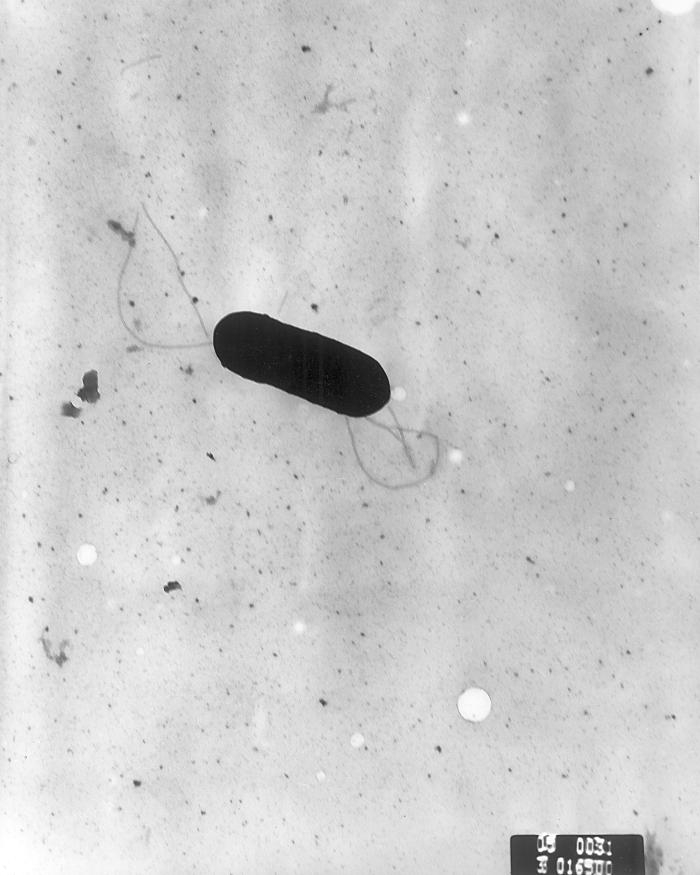
Listeria monocytogenes is an opportunistic pathogen
L. monocytogenes can be found in vegetation, raw foods, soil, water, animal faeces and, in some cases, food processing environments. It is an opportunistic pathogen with genetic mechanisms for survival and can last longer under adverse conditions than any other non-spore forming bacteria.
Unlike most other pathogenic bacteria, L. monocytogenes is able to grow at temperatures as low as 1°C and studies show that the rate of growth can double at 8°C compared to 5°C. Reports indicate that failure to sustain the cold chain was a contributory factor in many outbreaks of listeriosis in hospitals, which is why it is critical to maintain low temperatures to reduce the risk of further cases.
Biofilm formation, a layer of microorganisms adhered to a surface, is a particular feature of L. monocytogenes. Biofilm allows L. monocytogenes to survive and persist for long periods, including on food-contact surfaces. Once established, they are known to remain on surfaces for up to seven years due to their resistance to chemical disinfectants, meaning they can easily contaminate food that comes into contact with the biofilm, which could cause big problems for manufacturers.

What exactly is listeriosis?
Listeriosis is a bacterial infection that can be either invasive or non-invasive and has an incubation period of up to 90 days. In most healthy people, listeriosis is non-invasive and leads to a mild fever and gastroenteritis with symptoms passing within three days without the need for treatment.
Invasive listeriosis can be more severe and is most often found in the elderly, pregnant women, unborn or newly delivered infants and those with a weak immune system. The most common symptom of listeriosis reported by Public Health England in 20151 was bacteraemia followed by meningitis. Other symptoms include encephalitis, miscarriage and long-term health problems.
Who is at most risk from contracting listeriosis?
Listeriosis has traditionally been associated with pregnant women and their unborn or new born babies, and campaigns for foods to avoid during pregnancy have been successful. There remains perhaps less awareness of other vulnerable groups, especially the elderly and those with a weakened immune system. Public Health England concludes in a report1 published in 2015 that malignant cancers or tumours (26.3 per cent) were the most common underlying condition for cases of listeriosis in England and Wales in 2014, followed by auto-immune diseases (16 per cent), such as arthritis or Crohn’s disease.
What foods are most commonly associated with listeriosis?
L. monocytogenes has been found in a variety of foods and is most commonly associated with chilled, ready-to-eat foods. These foods are higher risk due to there being no way to destroy the organism during the food processing system, possible exposure to post food processing contamination and the nature of their long shelf-life. Food types that have most commonly been implicated in outbreaks of listeriosis are:
- Pre-prepared foods: pre-packed sandwiches, prepared salads
- Meat: cooked sliced meats, paté
- Fish: smoked salmon, cooked shellfish
- Dairy: soft blue veined cheeses, mould-ripened soft cheeses.
Hospital-related outbreaks between 2003 and 2014 (10 outbreaks) found pre-packed sandwiches were implicated in most cases.
Key controls to prevent outbreaks of listeriosis
The FSA has developed a range of food safety management packs for different sectors of the food industry to help food business operators manage their food safety management procedures. Enforcement officers also check that businesses have appropriate HACCP-based food safety management systems in place.
However, there are two main methods to control L. monocytogenes:
- Control of growth
Growth of any L. monocytogenes that may be present on high risk ready-to-eat foods must be minimised to prevent the bacteria reaching harmful levels. This can be achieved by applying effective time and temperature controls:
Maintain the cold chain: Maintenance of the cold chain at 5°C or below is good practice (compared to the legal requirement of 8°C).
Shelf life: Businesses that prepare their own food onsite should set their own appropriate shelf life. Other outlets should follow the manufacturer’s instructions for use by dates and storage.
- Avoid contamination
Procedures to prevent contamination of food by L. monocytogenes from its various sources are:
Cleaning and disinfection: High standards are important to remove any potential sources of L. monocytogenes and to prevent formation of biofilms.
Personal hygiene: As food handlers may be carriers of L. monocytogenes, high standards of personal hygiene (such as handwashing) are important.
Cross-contamination: Closely following and adhering to FSA E.coli O157 control of cross-contamination guidance will help to minimise risks from L. monocytogenes.
Procurement / purchase: A clear policy should be in place for the procurement / purchase of higher risk ready-to-eat foods to ensure that they are only bought from reputable suppliers who have controls for L. monocytogenesin place.
The risk for vulnerable consumers contracting listeriosis is avoidable if these appropriate controls are in place and effectively managed. STS is a food safety consultancy that works alongside the leisure and hospitality, retail and health sectors, including hospitals, where it implements training, audits and frameworks.
To find out more about food safety and outbreak prevention, visit http://www.sts-solutions.com/
References:
- Public Health England (2015) Listeriosis in England and Wales in 2014: summary report [online] Public Health England. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/406015/hpr0615_lstria.pdf [cited 9 June 2015]
- European Food Safety Authority (2015) Campylobacteriosis cases stable, listeriosis cases continue to rise, say EFSA and ECDC [online] European Food Safety Authority/ Available at: http://www.efsa.europa.eu/en/press/news/150128.htm [cited 9 June 2015]
Fiona Sinclair is the director at STS, a UK-based food safety consultancy and training provider.


2 thoughts on “Listeriosis: a major concern for public health?”