The Carbapenem-Resistant Enterobacteriaceae (CRE), or “nightmare bacteria” as CDC director Dr Tom Frieden once called them, is not unique to the Ronald Reagan UCLA Medical Center, despite all the media coverage.
Since first being detected in a North Carolina hospital in 2001, only Maine, Idaho and Alaska have not reported a confirmed CRE case caused by the KPC enzyme and about a third of states have reported CRE cases caused by the NDM enzyme.
In fact, according to a report by Charlotte, NC press, the Carolinas HealthCare System- Lincoln (CHS) has reported 3 cases since the beginning of the year.
In a statement from the CHS they say, There have been three cases identified at Carolinas HealthCare System Lincoln this year – two of which were acquired outside of the hospital.
CHS is aggressively addressing this issue, including using decontamination procedures and protocols that go beyond industry standards.
In a press briefing in 2013, CDC director, Dr. Thomas Frieden said the following about CRE:
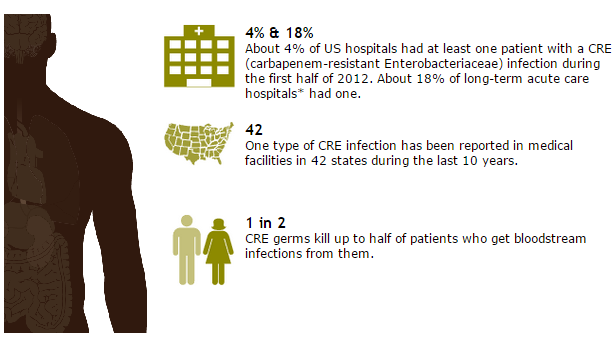
What I’m talking about today is CRE, carbapenem-resistant enterobacteriaceae. CRE are nightmare bacteria. They pose a triple threat. First, they’re resistant to all or nearly all antibiotics. Even some of our last-resort drugs. Second, they have high mortality rates. They kill up to half of people who get serious infections with them. And third, they can spread their resistance to other bacteria. So one form of bacteria, for example, carbapenem-resistant klebsiella, can spread the genes that destroy our last antibiotics to other bacteria, such as E. coli, and make E. coli resistant to those antibiotics also.
To give you some background, the long word, carbapenem-resistant enterobacteriaceae, is a family of more than 70 different kinds of bacteria. It includes some very common ones, like klebsiella and E. coli,that are normally present in our intestines. Sometimes, however, these bacteria can get into the wrong places like the blood or the bladder. When this happens, people can get severe infections called urinary tract infections. Some types of enterobacteriaceae have become resistant to antibiotics, even high-powered, last resort, last line of defense of antibiotics, called carbapenems. Antibiotic resistance is what turns normal enterobacteriaceae into drug resistant or CRE. Now there are many different types of resistance that are carried by different plasmids that go by names like KPC or VIM or NDM, or CRKP. These are all types of CRE. Types of resistant bacteria. They all result in the same end point, a highlydrug-resistant infection that has a very high fatality rate for people who have serious infections with it.
The risk of CRE infection is highest among patients who are getting complex or long-term medical care. This mostly means patients in regular hospitals or long-term acute care hospitals, or nursing homes. CRE spread among people, mostly patients in hospitals and long-term care facilities, usually from unclean hands. Medical devices such as ventilators or catheters increase the risk of life-threatening infection because they allow new bacteria to get deeply into a patient’s body.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | RSS


One thought on “CRE ‘nightmare bacteria’ not unique to UCLA”