In the previous post about sexually transmitted infections (STI), we looked at the more well know and common infections. In this second part, we will look at those infections less well known and in some cases, pretty uncommon.
Trichomoniasis

The CDC estimates about 3.7 million new and existing infections of this parasitic STI (Trichomonas vaginalis).
This STI, unlike the others, is seen in individuals 25 years of age and up. Trichomoniasis is considered the most common curable STI; however, only about 30% develop any symptoms.
Trichomonas vaginalis is the most common pathogenic protozoan infection in humans in developed countries.
It is spread through contact with vaginal and urethral discharges during sexual intercourse. It is highly unlikely to catch this parasite by means of sitting on a toilet seat as many believe; Trichomonas just does not withstand drying and do not survive very long in the environment outside of the host.
In women, though sometimes asymptomatic, when symptoms are present it is characterized by a profuse, thin greenish-yellow discharge with a foul odor. Other signs of trichomoniasis are small hemorrhages causing reddening on the cervix known as “strawberry cervix”, vaginal itching and an urge to urinate.
In men, most show no symptoms, however it may invade the prostate and seminal vesicles.
Rarely, babies born to infected mothers may contract infection during delivery.
It usually takes about a week after infection before symptoms appear, but many people are symptom-free carriers for years.
Trichomonas often coexists with gonorrhea; in up to 40% of people with gonorrhea have a concurrent trichomonas infection. It is also seen in women that also have bacterial vaginosis. So a full STI check must be done if someone is diagnosed with trichomoniasis.
This infection is typically diagnosed based on finding the motile parasite by microscopic exam of discharge material or by culturing the parasite. It has been seen in PAP smears; however this must be confirmed by a different test.
Trichomonas can be treated with the antibiotic metronidizole or tinidazole. Sometimes treatment may fail and you will usually be treated with the same drug for a longer time at a higher dose. All sexual partners should be treated at the same time to prevent the “ping-ponging” effect of reinfection. You do not build any immunity to this parasite, so you can get reinfected.
Lymphogranuloma venereum (LGV)
Also known as Lymphogranuloma inguinale and tropical bubo, Lymphogranuloma venereum (LGV) is a sexually transmitted chlamydial infection caused by three related but distinct types of Chlamydia trachomatis (L-1, L2 and L-3).
These are different than the types that cause non-gonococcal urethritis/cervicitis in men and women respectively.
Though LGV is more common in tropical and subtropical parts of the world; it is seen in outbreaks in the United States and Western Europe particularly in men that have sex with other men.
This bacterium is transmitted primarily through sexual contact (oral, genital or anal) and with any direct contact with open lesions. It is believed to be transmissible via skin to skin contact.
The infection is characterized by small painless papules, nodules or ulcers which may form on the penis or within the urethra in men, and on the vulva, vaginal wall or cervix in women. This lesion frequently may go unnoticed. It may take from 3-30 days before the primary lesion appears.
Lymph nodes in the area near the infection typically swell and the presence of inguinal or femoral buboes may be seen. In women these external node are rarely affected, but proctitis may be the result of swelling of the pelvic nodes extending to the rectum.
For those that practice rectal intercourse, proctitis may be a manifestation of the disease. Rectal ulcers, discharge, pain and bleeding are also common presentations.
Elephantiasis of the genitals in both men and women may occur in cases of untreated LGV.
Like other ulcer forming sexually transmitted infections (STI) like syphilis, chancroid and herpes; LGV increases the chance of getting HIV.
Chancroid
Also known as soft chancre and ulcus molle, chancroid is an acute, sexually transmitted infection caused by the bacterium, Haemophilus ducreyi or Ducrey’s bacillus.
It is characterized by single or multiple painful ulcers that bleed on contact. The ulcer or sore begins as a tender papule that becomes a pus-filled, open sore with eroded or ragged edges. It is soft to the touch, unlike a syphilis chancre that is hard.
The chancroid ulcers are more commonly found in uncircumcised men, on the foreskin or in the groove behind the head of the penis.
The lesions are frequently accompanied by painful, swollen lymph nodes in the region.
In women, lesions may occur on the inner and outer vaginal lips, the vaginal wall or cervix. Asymptomatic cases in women do happen.
Chancroid is most prevalent in tropical and subtropical developing countries. It is much less common in temperate zones like the United States. When it is seen in outbreaks in industrialized nations, it is typically found among foreign travelers, migrant workers and those who are clients of sex workers.
The organism is transmitted by direct sexual contact with the discharges from open lesions or pus from buboes.
The incubation is from 3 to 5 days average, up to 14 days. The infection is transmissible in the primary lesion from weeks to months without treatment.
Chancroid is treatable with antibiotics (ceftriaxone, erythromycin or azithromycin).
Molluscum Contagiosum
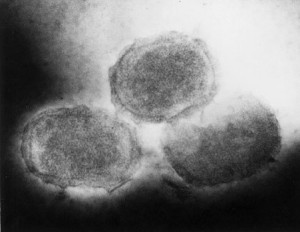
This is a viral infection of the skin caused by a poxvirus. It results in lesions that are smooth, firm and spherical ranging in size from 2-5mm. The lesions may be yellow, white or flesh colored. They may show an indentation at the top of the lesion.
This infection is most frequently seen in children where the lesions appear on the face, trunk and extremities. In adults it is usually associated with being a sexually transmitted infection with lesions seen on the lower abdomen, genitalia or inner thighs.
Immunocompromised people tend to develop hundreds of disseminated lesions over the body and face. This may be explained by scratching of the lesions (autoinoculation).
Molluscum contagiosum is usually spread through direct contact, sexual or non-sexual. Non-sexual transmission is often through inanimate objects such as toys, doorknobs and faucet handles. Scratching and shaving over lesions can cause it to spread through autoinoculation. It is found worldwide.
In immunocompetent people the viral infection will usually resolve itself within two years at the high end.
In adults, removal of lesions is frequently recommended to shorten the length of the disease. This can be done by scraping, freezing or laser therapy. There is no medicinal treatment that satisfactorily treats the infection.
Diagnosis can usually be made clinically. Confirmation can be made by examining the lesion microscopically for classic “molluscum” or “Henderson-Paterson bodies”.
Prevention of molluscum contagiosum is through avoiding skin contact, particularly sexual contact with an infected person. Also not sharing personal items like bath towels and sponges will help prevent infection. To avoid spreading lesions and autoinoculation, do not scratch or shave over lesions.
Sexually Transmitted Infections: Those common and those not so common, Part 1
Robert Herriman is a microbiologist and the Editor-in-Chief of Outbreak News Today and the Executive Editor of The Global Dispatch
Follow @bactiman63


Use latex condoms the right way every time you have sex. This can lower your chances of getting trichomoniasis. But the parasite can infect areas that are not covered by a condom so condoms may not fully protect you from getting trichomoniasis.