NewsDesk @bactiman63
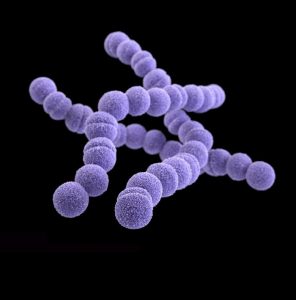
The Argentina National Ministry of Health has been monitoring invasive group A streptococcus since 2018. Streptococcus pyogenes is a Gram-positive bacterium and is the most frequent bacterial cause of acute pharyngitis and skin infections such as impetigo, cellulitis and scarlet fever.
During 2023, the National Health Surveillance System (SNVS) was notified of 118 confirmed cases of invasive infection by Streptococcus Pyogenes throughout the country, of which 16 died. The provinces with the highest number of confirmed cases accumulated in 2023 are Buenos Aires (35), Santa Fe (20), Chubut (10) and Tierra del Fuego (10).
In relation to confirmed cases of invasive infection by Streptococcus pyogenes in previous years (2019-2022), the highest number of cases had been registered in 2022 with 75 reported cases. The number of cases in 2023 represents an increase of 281% over the same period in 2019.
It should be noted that this happens in the international context in which on December 8, 2022, the World Health Organization (WHO) reported that at least five Member States of the European region (France, Ireland, the Netherlands, Sweden and the United Kingdom of Great Britain and Northern Ireland) had reported an increase in the number of cases of invasive disease caused by group A streptococcus (Streptococcus pyogenes) and on December 19, 2022, the Pan American Health Organization (PAHO) also issued a communicated due to an increase in cases registered in Uruguay.
Subscribe to Outbreak News TV on YouTube
As mentioned, Streptococcus pyogenes, also known as group A Streptococcus, commonly causes mild illnesses such as tonsillitis, pharyngitis, impetigo, cellulitis, and scarlet fever. However, on rare occasions, the infection can lead to invasive disease that can cause life-threatening conditions and is responsible for more than 500,000 deaths annually worldwide.
Transmission occurs through close contact with an infected person and can be transmitted through coughing, sneezing, or contact with a wound.
The incubation period for the disease varies according to the clinical presentation, between 1 to 3 days. Treatment of infected persons with antibiotics for at least 24 hours usually eliminates their ability to spread.
Pharyngitis is diagnosed by bacterial cultures and is treated with antibiotics. Hand hygiene and personal hygiene can help control transmission.
For these reasons, the Ministry of Health of the Nation issues the following recommendations to the population.
The symptoms of pharyngitis are sore throat; fever; headaches; abdominal pain; nausea and vomiting; redness of the pharynx and tonsils; bad breath; enlarged nodes in the neck.
Regarding scarlet fever, the most frequent symptoms are a red and sore throat; fever (38.3 °C or more); red rash with sandpaper texture; deep red skin in armpit, elbow, and groin folds; whitish coating over tongue or back of throat; “raspberry” tongue; headache; nausea or vomiting; swollen glands; body aches.
In the presence of some of these symptoms, it is important to avoid self-medication with antibiotics and to consult a doctor for a timely diagnosis.
In the case of receiving a medical indication for antibiotic treatment, it is essential to complete the scheme (do not shorten or abandon treatments early), since the inappropriate use of antibiotics promotes bacterial resistance, a fact that threatens their effectiveness in the future.
Sick people should avoid going to public places (work, school) and restrict household contacts. It is also important to wash your hands frequently; Do not share objects for personal use (cutlery, glasses, towels, among others) and adequately and regularly ventilate the environments.
Finally, the national health portfolio additionally reminds that all people must have up-to-date influenza and COVID-19 vaccination, especially those with risk factors.
In this way, pregnant people should receive the flu or influenza vaccine in any trimester of pregnancy (in case of not having been vaccinated during pregnancy, the mother must do so within 10 days after delivery); boys and girls from 6 to 24 months, who must be given 2 doses separated by at least 4 weeks if they have not previously received two doses of influenza vaccine (those who do have at least two doses of influenza vaccine should receive only one dose).
Risk groups also have a vaccination prescription: people from 2 to 64 years of age who present certain conditions such as respiratory and heart diseases; diabetics; congenital or acquired immunodeficiencies (not oncohematological); people with obesity oncohematological patients and transplant recipients; cohabitants of oncohematological patients; people with chronic renal failure on dialysis or with expectations of entering dialysis in the following six months; people with severe developmental delay in children under 18 years of age; those who maintain chronic treatment with acetylsalicylic acid while under 18 years of age; people with genetic syndromes; with neuromuscular diseases with respiratory compromise and severe congenital malformations and cohabitants of premature infants weighing less than 1,500 g, among others. all the above,
Meanwhile, against COVID-19, people with a high risk of serious illness and complications, that is, people 50 years of age or older, should receive the primary schedule and booster doses every 6 months; people with immunocompromised and pregnant people. For their part, people with intermediate risk, that is, under 50 years of age with non-immunosuppressive comorbidities (chronic diseases and obesity), should receive the primary scheme, a booster dose at six months and then an annual booster dose; health personnel and strategic personnel. Finally, those with low risk will receive a full primary schedule and an annual booster, that is, people under 50 years of age without comorbidities.
- Afghanistan: Crimean-Congo Hemorrhagic Fever cases top 400 in 2023
- Anthrax outbreak update: 27 confirmed cases in bison in NWT
- South Africa: 10 additional measles cases reported in past week
- Dengue in Bangladesh: Cases top 12,000 for the year, 2 additional deaths reported
- California: First Human Case of St. Louis Encephalitis Virus Confirmed in Kern County
- Kentucky: Increase in Legionnaires’ disease reported in Lexington
- Italy: 5 dogs, cat test positive for H5N1 avian influenza in Brescia, according to media report


